Introduction
Rectal perforation without fistulization to the urethra is a serious complication of seed brachytherapy for prostate cancer that is very rare, with only two cases reported in the literature describing rectal perforation at 16 months1 and seven years2 after radiation.
We report a case of a contained rectal perforation 19 years after seed brachytherapy for prostate cancer.
Case Description
A 90-year-old man with multiple comorbidities that included Alzheimer’s disease, chronic obstructive pulmonary disease, and prostate cancer treated with permanent prostate seed brachytherapy 19 years prior, presented to our emergency department after a fall at home following several days of general weakness and lower abdominal pain.
On physical examination of the abdomen patient had mild tenderness across the lower abdomen and thoracic spine tenderness.
On presentation he was afebrile, normotensive, with sinus tachycardia. His lactic acid level was 6.1 mmol/L (normal range 0.5 – 1.8) and the white blood cell count was 15.6 K/cmm (normal range 4.5 – 10.0) without a neutrophil left shift. The remainder of the blood counts and chemistry were normal. He was also found to be in urinary retention without a urinary tract infection.
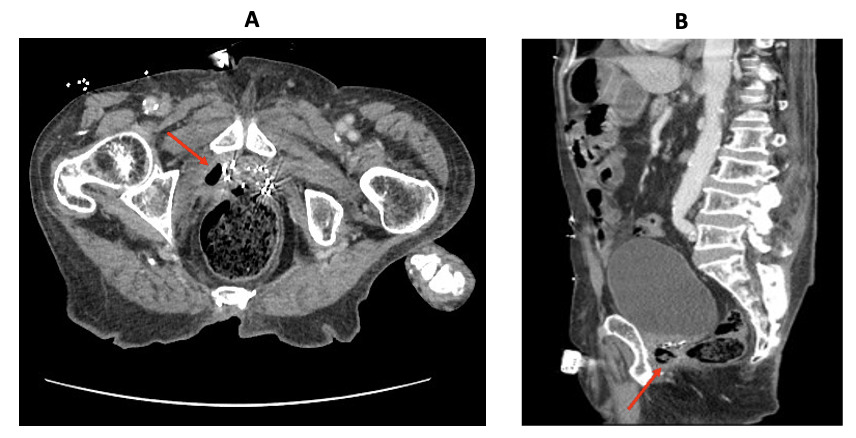
A non-contrast computed tomography (CT) scan of the abdomen obtained in the emergency department showed gas anterior to right aspect of the distal rectum at the level of the prostate radiation seeds without an abscess or inflammatory changes, suggestive of a contained rectal perforation. (Figure 1).
Additional imaging findings included T11 vertebral body fracture, left lower lobe lung consolidation, distension of the urinary bladder, and significant stool burden in the large bowel.
Upon admission to the hospital, patient was started on antibiotic therapy (Ceftriaxone) for community-acquired pneumonia, his T11 fracture was managed with a brace, and his constipation was treated with stool softeners.
The management of the contained rectal perforation was discussed in a multidisciplinary fashion involving the patient family members and the General Surgery, Urology, Radiation Oncology, Palliative Care, and the Medicine teams.
While the contained perforation was considered to be related to the brachytherapy seeds, a decision was made to not perform any surgical intervention based on the contained nature of the perforation in the retroperitoneum, lack of an associated abscess, and more importantly, respecting the patient’s and his family clear wishes to maximize medical management and avoid any additional tests that were recommended (barium enema or a proctoscopy) or surgical interventions.
The patient improved clinically; his lower abdominal pain resolved, and he continued to tolerate a regular diet and move his bowels. He was discharged to home after a 20-day stay in the hospital and was doing well on a follow-up visit three months later.
Discussion
Brachytherapy is an increasingly used treatment modality for prostate cancer and has a lower complication rate than external beam radiation.1,3 This is true of both early (6% versus 44%) and late (2% versus 22%) complications.1 However, brachytherapy does carry some risk, and both clinicians and patients should be familiar with these and engage in shared decision-making regarding optimal treatment.
Early complications of brachytherapy include proctitis (75%) and cystitis (20-80%), in addition to rectal pain and fecal urgency, while late complications include erectile dysfunction in up to 73% of patients, urinary incontinence (45%), bowel symptoms (4-9%), chronic proctitis (5%), and urethral strictures (1-2%).1,2,4,5 While rectal perforation is an extremely uncommon complication,6,7 there are reports of rectourethral fistulas after brachytherapy seed implantation, with incidence rates of 0.2%-0.7%.2,8,9
Given the paucity of literature describing isolated rectal perforation, there is not a defined pathophysiologic pathway by which this occurs. However, we postulate that it may be similar to the pathophysiology encountered in the development of rectourethral fistulas after brachytherapy seed implantation. For these patients, most literature describes the inflammation promoted by rectal biopsies as the most significant risk factor for fistula formation,9,10 though one study also notes short prostate to rectum distances as a risk factor for fistulization.11
In the two reports of isolated contained rectal perforations in this setting, symptoms were described as anal pain and discharge in one patient, and hematochezia in the other.6,7 In rectourethral fistulas, similar symptoms are observed, with the addition of fecaluria, pneumaturia, passing urine per rectum, and urinary tract infections.3,12 Our patient was somewhat unique in his presenting symptoms, with malaise and abdominal pain, but no rectal pain or blood per rectum to suggest a localized rectal pathology.
In our case, it should be noted that, due to patient preference, further invasive workup was not completed, and the diagnosis of isolated contained rectal perforation was based largely on imaging. Therefore, it is possible that an occult rectourethral fistula could have been present. However, the lack of local inflammation on imaging, the absence of a urinary tract infection, and the lack of recurrence despite not undergoing a fecal diversion argues again this possibility.
To our knowledge, there are only two described cases of isolated rectal perforation attributed to prostate seed brachytherapy (in the absence of a rectourethral fistula). Both were managed with fecal diversion.6,7 Rectourethral fistulas, which likely occur through similar pathophysiologic processes, provide a template for the management of isolated contained rectal perforation. The vast majority of patients with a rectourethral fistula secondary to prostate seed brachytherapy are managed initially with fecal diversion.2,3,7,8,12–15 Some surgeons also perform urinary diversion at the time of ostomy creation.12,13,15 Most are then managed with surgical primary closure of the fistula, with many surgeons opting for additional flap repair, which can be anorectal advancement flaps, omental, or gracilis flaps.8,12–14,16 The time frame from diversion to fistula repair is not well described, with the literature reporting a range of 5-43 months.3 Rates of ostomy reversal are also poorly described, with one study noting that only 15% of patients had intestinal continuity at the conclusion of their treatment.15 Fortunately, management with fecal diversion (with or without urinary diversion) followed by definitive fistula management as described above, has good success rates, with significant symptomatic improvement and negligible fistula recurrence.3,7,8,13,15,16
Consideration for patient preference and the input of all involved medical and surgical specialties is paramount in ensuring appropriate care. Though previously described cases of brachytherapy-related isolated rectal perforation and the related pathology of rectourethral fistula have been managed with fecal diversion, this is not necessarily mandatory, particularly in the case of isolated contained rectal perforation. We suggest that in highly comorbid and elderly patients, consideration of nonoperative management for isolated, contained, brachytherapy-related rectal perforation is warranted, especially considering patient-related factors such as quality of life and independence, which would be significantly impacted by major operations such as fecal diversion. Indeed, our patient, managed expectantly, demonstrated significant improvement in his generalized symptoms, and has not had any adverse effects. This is supported by one prior literature review, which, though focused on post-brachytherapy rectal bleeding, which our patient did not have, recommends lifestyle modification and conservative management in order to minimize perforation risk.10
Conclusion
Brachytherapy for prostate cancer is an increasingly used treatment modality, and rare, late-onset complications are still being elucidated. We describe the third known case of isolated, contained rectal perforation attributed to prostatic brachytherapy seed implantation. Unlike the previous two cases, our patient was successfully managed nonoperatively. In future such cases, we advocate for consideration of patient lifestyle, comorbidities, and treatment preferences in determining whether major operative repair, medical management, or both are indicated.